
The COVID-19 booster.
The science is there … but so is the opportunity for Big Pharma to make billions.
“Public”is the operative term in public health — it’s what we do collectively to assure conditions for people to be healthy. “Public” implies collective action; we, as a society, doing what we could not do alone. The principal agent of the public in a democratic society is our government, chosen by the people for the people to act on our behalf to promote public welfare. Good roads, clean air, public parks, public safety — these are all things we leave to our government to do for us. Public health is, perhaps, the center of all of them. After all, without our health, what more do we really have?
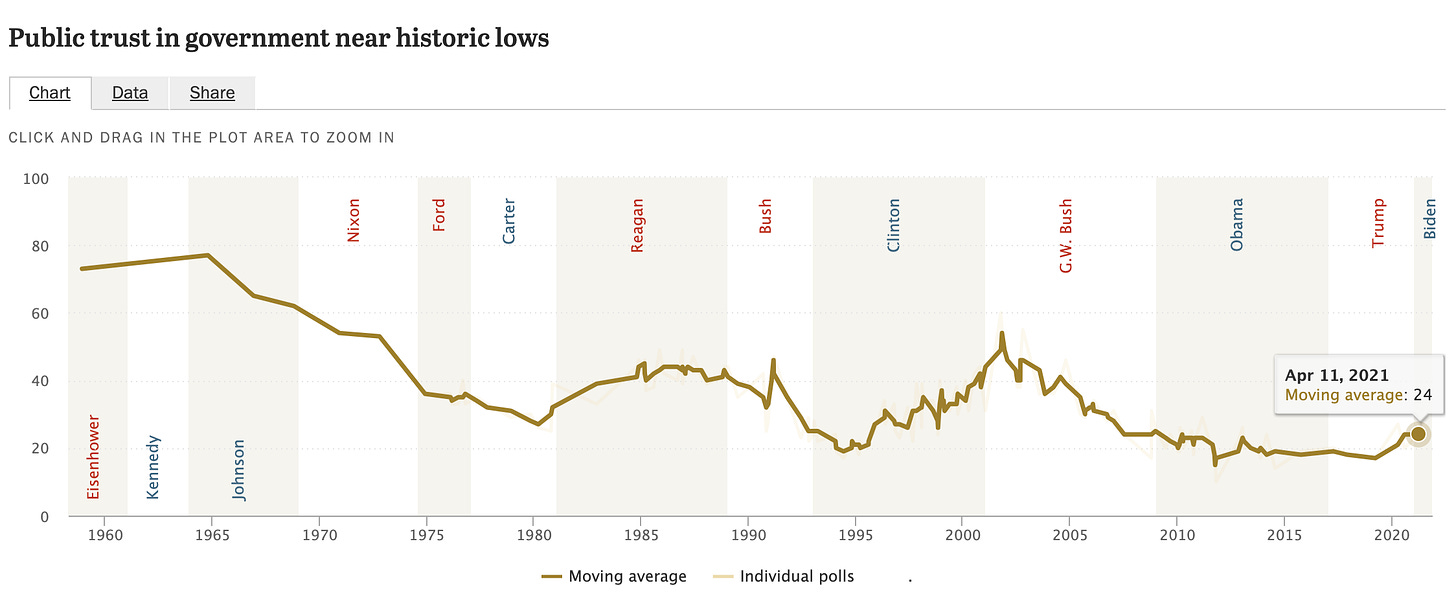
And yet our response to this pandemic has been bedeviled by a startling lapse in public action. Whereas our counterparts in places like New Zealand, Australia, Canada, and even the U.K. have suffered far fewer cases, hospitalizations, or deaths because of incisive and timely action to reduce spread, we have not. That’s because public action requires public trust — the belief that the government is truly working on our collective behalf, taking correct actions to protect us all. And public trust is near an all time low. During the Eisenhower era, 73% of Americans believed they could trust the government to do what was right most or all of the time. Today, only 24% do.
On social media, that loss of trust has been weaponized by a small minority to sow conspiracy and doubt in any public action against the pandemic.
I honestly thought that where our failed public trust had flummoxed our mitigation efforts, our technology — in the form of the medical marvel of a vaccine — would save us. I thought that the advent of a vaccine, something each could do on their own, would ultimately end this. And yet I forgot that the choice to be vaccinated was, itself, a function of public trust. So here we are: barely half of eligible people are fully vaccinated.
And this is where I get to the vaccine boosters.
On Wednesday, the Biden administration announced a policy of recommending a booster shot for fully vaccinated Americans eight months after their second dose beginning in September pending U.S. Food and Drug Administration approval. Though the decision is backed by decent science … it’s backed by something else too.
The Science.
The Centers for Disease Control and Prevention published three studies in their weekly Morbidity and Mortality Weekly Report. The first is a study of 1,129 patients who had been given two doses of mRNA vaccine (Pfizer or Moderna) over 24 weeks beginning in March. It found that the effectiveness against hospitalizations was 86% over the first 12 weeks, and barely budged to 84% over the second 12 weeks. This study establishes that the vaccines don’t wane in effectiveness against hospitalizations over time (or, given the study period, against the delta variant).
The second study, also based in New York, looked at age-adjusted hospitalization and infection among people vaccinated with the mRNA vaccines. It confirmed that while hospitalization risk was similar over time, infection risk increased among vaccinated people, dropping the vaccine effectiveness against infection from 91.7% to 79.8%.
Finally, the third studied residents of nursing homes between March and August of this year. That study found that while two-dose mRNA vaccines were 74.7% effective against infections in nursing homes between March and May, effectiveness declined to just 53.1% between June and August. Taken in the context of the other two studies, it suggests that baseline effectiveness in seniors of the two-dose mRNA regimen may be lower in more vulnerable people, and that the impact of delta in these communities is more pronounced.
There’s other data that is worth considering from abroad, as well. An Israeli HMO compared risk of infection among nearly 150,000 people over 60 who had received a third dose of mRNA vaccine at least one week prior with approximately 676,000 people who had not. The risk of infection was over six times higher among those who hadn’t yet received a third dose.
What does all of this mean?
Two doses remain highly effective against severe infection requiring hospitalization. However, protection against breakthrough infection may wane with time and, in the face of delta, particularly in older and more vulnerable people. It appears that a third dose — a booster — may help prop up waning effectiveness.
What we don’t know is if the booster will demonstrably reduce transmission by vaccinated people. Indeed, previous CDC guidelines recommending that vaccinated people mask up in communities with substantial transmission is based on the finding that infected vaccinated people can carry high levels of delta in their nasopharynx. Presumably, reducing breakthrough transmission reduces this possibility — but what does that mean for overall transmission patterns among the vaccinated?
The ethics.
Now for the benefits and costs. Remember that whole civics lesson about public action I led with? It comes back into play here. The individual benefits of a third dose seem clear: better protection against the risk of infection. The individual costs? Well, if you had that cold-like syndrome after your second dose, you’ll probably get it again after the third.
But what about the collective? If there were definitive evidence that the booster reduced transmission, you could argue that boosters would have a clear collective benefit. But there’s not, it’s just presumptive.
The collective costs are glaring. Billions of people in the world have yet to get a first vaccine — not because they have chosen not to get it, but because there simply isn’t any to go around. Indeed, the World Health Organization Director-General Tedros Adhanom Ghebreyesus proposed a moratorium on boosters until at least 10% of the citizens in every country are vaccinated.
Protecting unvaccinated people from the ravages of COVID-19, which is rampaging in parts of Africa right now, must be an end unto itself. Nevertheless, there’s also the domestic implications of a global pandemic. Don’t forget the origin story of delta. It evolved in India, leading to a massive surge there that killed thousands of people. It’s now menacing the rest of the world and all of us here in the US.
Lambda, delta’s heir apparent, has already emerged in Peru, with thousands of cases being reported across South America. Our failure to vaccinate the globe simply increases the probability that the next variant and the variant after that will emerge. Vaccine boosters mean that hundreds of millions of doses that could have gone toward vaccinating people who have not gotten a vaccine abroad will now go to offering boosters to double vaccinated people here at home.
But there’s another consequence. If we step back here, it’s clear that the most important question facing vaccinations isn’t whether to give double vaccinated Americans a third dose, it’s how to get unvaccinated Americans to take their first two. In that regard, our mantra has been that vaccines are safe and effective. Recommending a third dose implicitly undercuts our own arguments among these people, who’ll wonder how effective it really is if they need a third dose. The obvious counter argument here is that we’re dealing with a new variant, et cetera, et cetera … but if logical arguments were effective, they’d be vaccinated already. The choice not to vaccinate is fear-based and emotional. These new recommendations could embolden those feelings.
Here’s where I sit. I don’t think offering third doses was the best policy choice for us as a collective. But because that choice is now a fait accompli, I think it’s wise for individuals to get their boosters considering that if you don’t take them, they’re unfortunately more likely to wind up in the trash than in arms abroad that need them.
The money.
Why are we doing this?
Pfizer and Moderna have been lobbying the government for some time to offer third booster shots based on evidence that antibody levels among vaccinated people waned with time. Though there’s no reason to doubt the science, don’t assume that pharmaceutical corporations were doing this simply out of altruism.
An additional booster means literally 50% more in revenue for vaccine manufacturers. Analysts forecast an additional $6.6 billion for Pfizer and $7.6 billion for Moderna in 2023, largely as a result of booster sales. That’s in addition to the $60 billion in sales through 2022. The additional revenue is particularly critical for Moderna, which, as a startup, relies on the revenue it makes on its COVID-19 vaccine for its market valuation.
“Doing well by doing good,” is what folks in the business world might label Pfizer and Moderna’s efforts here — at least folks in the part of the business world that can line up for a third dose. The rest of the world might ask how “well” they should expect to do, and for whom the “good” ought to be done.











I appreciate this! I was torn about getting the booster, considering the dearth of vaccines in the rest of the world. I figured not getting my shot wouldn't mean a person who needed it getting it, but I'm glad to have you confirm that!
Good thoughts. Thank You.
What do you think about the future? Namely, relatively low vaccination rates in the USA for free vaccines, and, the lack of vaccines around the world. If we continue like this, the virus continues to roll and create more mutations, and takes more and more lives.
What would be a remedy? It seems that a broad (political) spectrum of people in the US could support global vaccinations. Their reasons could be humanitarian or not. They could be motivated by the collapse in their regional economies.
What leverage is there to do this? What buttons need to be pressed?
TY, MG